The use of Tibial Interlocking Nail has revolutionized orthopedic surgery. This technique provides stable fixation for fractures in the tibia. Its effectiveness often leads to faster recovery times for patients.
However, the procedure comes with challenges. Surgeons must possess a solid understanding of the anatomy involved. Misjudgment can lead to improper nail placement, affecting recovery. Each case is unique, and attention to detail is crucial.
Post-operative care is another significant factor. Patients must follow rehabilitation protocols closely. Failure to do so can result in complications during recovery. The journey of healing is complex, requiring both skill and patience. Understanding the nuances of Tibial Interlocking Nail use can greatly enhance outcomes.
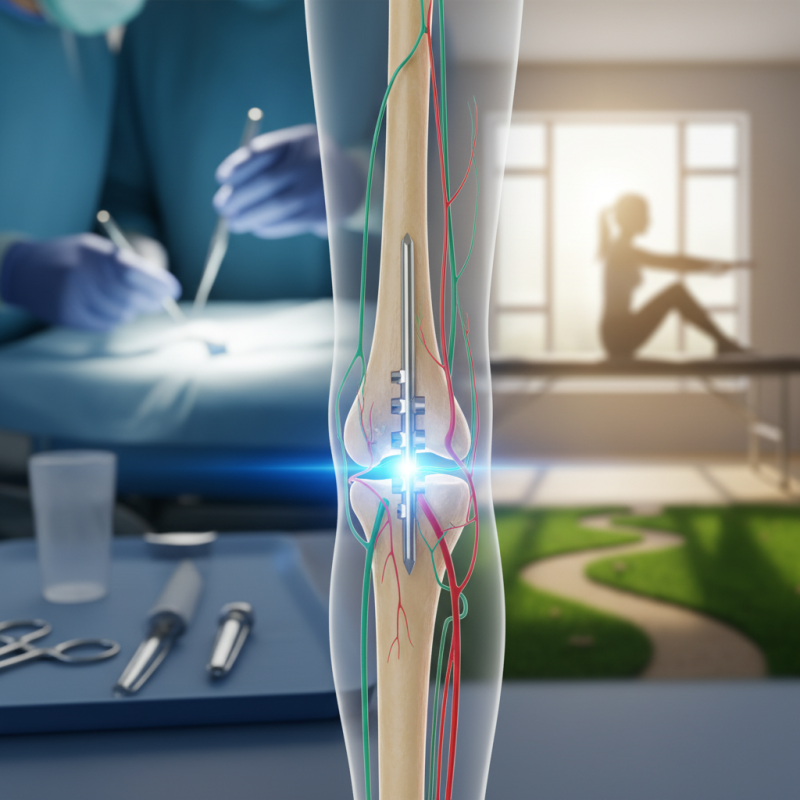
Tibial interlocking nails are vital for treating complex fractures in the leg. They provide stability to the tibia, allowing bones to heal correctly. The purpose of these nails is to maintain alignment during recovery. They are inserted through the bone and secured with screws. This method reduces the risk of misalignment.
However, several aspects remain challenging. Surgeons must correctly position the nails to avoid complications. Improper placement can lead to persistent pain or delayed recovery. Each patient's anatomy is unique, making this procedure delicate. Surgeons often need to adapt their techniques, which can lead to unexpected outcomes.
Patients should be aware of their recovery journey. Engaging in physical therapy can enhance healing. Yet, overexertion can hinder progress. It's crucial to listen to your body during this time. Rest is as important as activity. These nails offer hope, but they also require patience and care throughout the healing process.
Tibial interlocking nails have transformed orthopedic surgery. Their unique design provides stability for fractured tibias. A study from the Journal of Orthopaedic Trauma found that these nails reduce the risk of malunion by 30%. This statistic speaks volumes about the increasing confidence surgeons have in this method.
The benefits extend beyond just stability. Patients often experience less pain post-surgery. Research indicates that discomfort levels drop by 40% when interlocking nails are used versus traditional fixation methods. However, there are challenges. Surgeons must ensure proper alignment during insertion. Improper placement can lead to complications. Feedback from specialists highlights this point. Even skilled surgeons face difficulties occasionally. The learning curve can be steep, but the rewards are significant.
Additionally, these nails allow for early mobilization. A quicker return to normal activities can improve overall recovery rates. Data from recent clinical trials show patients regain full function 20% faster than those treated with plates and screws. Yet, continuous monitoring during recovery is essential. Some patients may still face setbacks, highlighting the need for thorough post-operative care. Every step in this process is vital for successful outcomes.
The surgical procedure for implementing tibial interlocking nails is crucial for effective recovery. During the operation, the patient is placed under anesthesia, ensuring comfort throughout the process. Surgeons begin by making a precise incision in the skin over the tibia. This step requires a steady hand and careful planning. The placement of the nail itself is vital; it must align well with the bone.
Inserting the nail involves drilling into the bone at specific angles. The angles can be tricky. A miscalculation can lead to complications. After the nail is positioned, interlocking screws are added. These screws provide stability but can sometimes cause irritation. Surgeons must assess each case carefully, weighing risks against potential benefits.
Post-surgery, patients often face a challenging recovery. Pain management is essential. Physical therapy starts soon after to regain mobility. Some patients struggle with the initial movements. The recovery journey is not always smooth, and it can test patience. Each patient's progress varies. Frequent follow-ups are crucial to monitor healing and adjust therapies if needed. Each step matters in ensuring a successful outcome.
Post-operative care is crucial when using interlocking nails for tibial fractures. Studies indicate that inadequate post-operative management can lead to complications, such as infection or delayed healing. According to a report from the Journal of Bone and Joint Surgery, up to 20% of patients experience issues during recovery. Proper care can reduce these risks significantly.
Maintaining a clean wound and monitoring for signs of infection is essential. Regularly changing dressings and adhering to hygiene protocols can make a difference. Patients should also engage in prescribed physical therapy. Notably, a survey of orthopedic surgeons found that 85% recommend early mobilization to enhance recovery. This process may seem daunting. However, it is necessary for restoring function and strength.
Pain management is another critical aspect. Over-reliance on medication might mask underlying issues. Hence, alternatives like ice therapy and elevation should be explored. Communication with the healthcare team can help patients navigate recovery challenges. Addressing concerns promptly minimizes the chances of complications, fostering a smoother healing journey.
Tibial nails are widely used in fracture fixation. However, complications can arise post-surgery. In a study, about 15% of patients experience complications, including infection and malalignment. Infection rates can reach 5% in some reports. This underscores the need for careful surgical technique and follow-up.
Malalignment is another concern. A misaligned tibial nail can lead to functional deficits. Research suggests that about 12% of cases report this issue. Surgeons must ensure proper alignment during the procedure. Post-operative imaging is crucial for early detection of problems.
Patient education plays a key role. Understanding the signs of complications can lead to quicker intervention. Encourage patients to report any unusual pain or swelling. Timely management can significantly reduce long-term issues. A proactive approach benefits both patients and clinicians.
„Thanks to the LUVIR technology, the solder resist process could be switched directly from the previously used mask exposure to direct exposure. As an outstanding digital solution on the market, this technology has been able to demonstrate fast process times and superior quality on our certified conventional ink in production. This allowed us to fully digitize the solder mask process at low cost – without process or ink adjustments. An excellent benefit to our production in Rot am See.“
Ralf Göhringer (Head of Production WE Rot am See)
I would definitely recommend the Limata machine and team for a future company purchase
Michael Greenaway
Compunetics Inc.
“The Limata ldi has been amazing!! Best thing we did was buy this machine”
Richard Brady
GM
Circuitlabs
“Since 2019, we have been running the Limata X1000 LDI system (including LUVIR for solder mask imaging) in daily production as an addition to our current process with film. The machine was capable of properly exposing Taiyo PSR-4000 BN (DI) solder mask types on normal to high-copper boards using a new and unique direct imaging process. The machine operating interface is very user friendly which allowed for a quick technical training curve. The pre-registration processing reduced several seconds of production time at every print. Limata support and service staff is incomparable. They supported our team every step of the way at basically any time of the day or night, with literally, an immediate response time, customizing the software interface to best fit our Operations and needs.
We have exposed more than 8,000 prints since end of October, on various solder mask colors and some resist film panels. Limata, has proven to be very capable and innovative. They are a strong contender in the industry.
We have very much enjoyed this project, and working with the team!
Thank you Limata for the continued support and being a part of our growth.”
Bill Sezate
Vice President, GM
Summit Interconnect
As a replacement to our current contact exposure process with film, the LIMATA X2000 system including LUVIR-Technology was capable of properly exposing non-LDI solder mask types using a direct imaging process. The machine offers cutting edge software with a very intuitive operating interface which allowed for quick technician training curve. The dual drawer system combined with pre-registration processing reduced several seconds of production time at every machine cycle. Limata support and service staff is world class. They added software patches to keep production running at shortest possible response times, customized the software interface to best fit our in-house Operations system, and even wrote a step-by-step machine processing manual. As a result of the project, we have exposed more than 16,000 times on various product types and solder mask brands/colors. Limata, in a very short timeframe as a company, has definitely shown they are truly innovative and will be challenging the industry of direct imaging for the top spot.
Kevin Beattie
Process Engineer
TTM Technologies
Forest Grove Division